Breast Reconstruction with Tissue Expanders
Choosing the Right Implant
Implant Feel
Choosing between silicone and polyurethane implants is crucial for those prioritizing feel and firmness. Silicone implants, known for their soft, natural feel, mimic breast tissue closely. They come in a silicone shell that patients often prefer for its realistic texture.
Polyurethane-coated implants, on the other hand, offer a firmer option. They adhere better to the body’s tissues, reducing movement post-surgery. This feature might appeal to individuals with a higher body mass index, where implant stability is key.
Risk Factors
Implant rippling and rupture are significant concerns in breast reconstruction. Silicone implants have a lower risk of rippling compared to saline options, due to their cohesive gel filling. However, they’re not immune to rupture.
Polyurethane implants have a unique advantage here. Their surface texture minimizes the chance of kinking or rippling, offering a smoother outcome under the skin. Yet, it’s essential to weigh this against the potential difficulty in detecting ruptures through imaging tests.
TGA Review
The Therapeutic Goods Administration (TGA)’s recent review has impacted implant choices available in Australia. It highlighted concerns over certain types of implants linked to rare conditions. This scrutiny ensures that only implants meeting strict safety standards remain on the market.
Patients must consider these factors alongside personal preferences and medical advice when selecting an implant technique. Whether opting for an immediate expander or evaluating prosthesis options, informed decisions lead to safer, more satisfying outcomes.
Preparing for Surgery
Health Optimization
To ensure a smooth surgery and recovery, patients must focus on health optimization. This includes stopping smoking well in advance of the procedure. Smoking can delay healing, increasing the risk of complications. Maintaining a healthy weight is also crucial. It helps minimize surgery risks and supports better outcomes.
Patients should follow their surgeon’s guidance closely. These pre-surgery steps are vital for those undergoing breast reconstruction with tissue expanders after an initial mastectomy.
Infection Prevention
Reducing infection risk is another critical preparation step. Patients should avoid shaving or waxing the surgical area before their procedure. Cuts can become entry points for bacteria, leading to infections.
Surgeons might also recommend specific antiseptic washes to use before coming to the hospital. Wearing clean clothes and using fresh gauze pads at home are simple yet effective measures to keep the area clean.
Blood Sugar Control
For patients with diabetes, controlling blood sugar levels is essential. High blood sugar can slow down healing and increase infection risks. Working with your healthcare team to manage these levels before and after surgery will help ensure a smoother recovery process.
Understanding the Operation Process
Pocket Creation
The reconstruction process begins with a crucial step. Surgeons create a pocket under the muscle. This space is for the tissue expander.
The expander is key to preparing the body for the final implant. It’s placed in a carefully prepared layer beneath the skin and muscle. This ensures the area can support the expansion process.
Skin Stretching
Next, comes the gradual skin stretching. This is vital for creating enough space for the final implant.
The expansion process involves injecting saline into the expander over weeks or months. This helps to increase the skin and muscle area gradually. Patients should expect several visits to their surgeon during this phase. Each visit allows for more saline to be added, slowly stretching the tissue.
Safety Measures
It’s important to note that not all implants and expanders are equal. The Therapeutic Goods Administration (TGA) has assessed and recalled certain products due to safety concerns.
Patients should seek detailed information from their surgeons about these assessments. Knowing which products are safe and approved adds an extra layer of security to the healing process.
Managing Post-Op Care at Home
Pain Management
After understanding the operation process, managing pain and discomfort is crucial. Patients should follow their surgeon’s advice on taking prescribed medications. Ice packs can also reduce swelling and soothe the area.
It’s important not to overdo activities that could strain the chest muscles. Rest is key for recovery.
Infection Signs
Spotting signs of infection early ensures timely intervention. Look out for increased redness, swelling, or pus around the incision sites. A fever above 100.4°F (38°C) or chills are red flags.
Patients must contact their medical team immediately if they notice these symptoms. Prompt action can prevent complications.
Wound Care
Proper wound care is vital for healing. Surgeons provide specific guidelines on how to care for incisions and when to change dressings. Keeping the area clean and dry helps prevent infection.
Avoiding direct water pressure on wounds during showers is recommended until cleared by the surgeon.

Activity Restrictions
Surgeons advise on what activities to avoid post-surgery. Lifting heavy objects or engaging in high-impact exercises can jeopardize recovery. Adhering to these restrictions ensures a smoother healing process.
Patients gradually resume normal activities based on their doctor’s guidance, ensuring safety and effectiveness in recovery.
Navigating Recovery and Activities
Gradual Return
After managing post-op care at home, planning for a gradual return to normal activities is crucial. It’s important to respect your body’s healing timeline. Your treatment team will guide you on the right time to resume daily tasks. Initially, strenuous activities should be avoided to prevent complications.
Patients often wonder when they can go back to work or engage in physical exercise. The answer varies based on individual recovery rates and the nature of their job or activity. Generally, light activities can be resumed within a few weeks, but it might take months before returning to more demanding tasks.
Follow-up Care
Regular follow-up appointments are vital for monitoring progress. These sessions with your care team help ensure that the expansion process is proceeding as planned and allows for any necessary adjustments in volume or size. They also provide an opportunity to address concerns like discomfort or rippling at the expansion sites.
During these appointments, your team will check for signs of infection, proper healing, and any potential complications related to breast reconstruction with tissue expanders. This ongoing treatment ensures optimal results and peace of mind throughout the recovery process.
Lifestyle Adjustments
Making lifestyle adjustments supports long-term health and surgical outcomes. This includes maintaining a healthy diet, avoiding smoking, and limiting alcohol consumption. Such choices not only aid in recovery but also enhance overall well-being.
These adjustments can significantly impact the success of breast reconstruction and reduce the risk of complications like large cell lymphoma, a rare side effect associated with certain types of implants.
Planning for Exchange Surgery
Surgery Timing
After navigating recovery and activities, planning the exchange surgery is crucial. This step involves replacing the temporary expander with permanent implants. Patients should have detailed discussions with their plastic surgeons about the optimal timing. Factors like healing from the initial surgery and expansion process impact this decision.
The timeline varies but often occurs several months after the first procedure. This allows the tissue expanders to stretch the skin sufficiently.
Expectations Setting
Setting realistic expectations is key. During consultations, surgeons provide insights on what to anticipate regarding appearance and sensation post-exchange. They also discuss potential risks, including infection or complications at drain sites.
Understanding these aspects helps in making an informed decision about proceeding with exchange surgery.
Implant Choices
Choosing implants is a significant step. Initial recovery and results from using tissue expanders may influence this decision. Patients might opt for a different size or material than initially planned.
Surgeons offer guidance based on aesthetic goals and physical health considerations. They ensure choices align with patients’ desires while maintaining safety protocols.
It’s essential to consider all options thoroughly before finalizing decisions on implant types.
Exploring Nipple Reconstruction Options
Surgical Techniques
After the exchange surgery from tissue expanders to permanent implants, many patients consider nipple reconstruction. This step can significantly enhance the appearance of the reconstructed breasts, making them look more natural. Surgeons may create a new nipple through various methods, including grafting and local flap techniques. These procedures aim to match the new nipple to the contralateral breast in terms of size, shape, and projection.
Patients should discuss these options with their breast team early on. This ensures a unified approach throughout the reconstruction process.
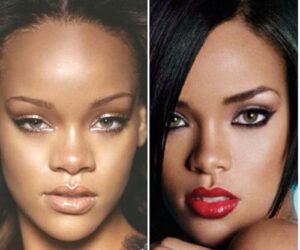
Tattooing Benefits
Another popular method for finalizing the look of reconstructed breasts is areola tattooing. Unlike surgical options, tattooing is less invasive and can be highly effective in creating a natural-looking areola. It offers precise color matching and can add depth and dimension to the breast form without additional scars.
Many find this method appealing for its simplicity and quick recovery time.
Timing Considerations
Timing is crucial when planning nipple reconstruction. It’s usually performed as the last stage of breast reconstruction, allowing the new breast to heal properly first. Discussing timing and procedures with your surgical team is essential for a smooth transition through each phase of reconstruction.
They will guide you on when your skin and tissues are ready for this final touch, ensuring optimal results for both appearance and health.
Addressing Complications and Risks
General Risks
Every surgical procedure carries its set of risks. Breast reconstruction with tissue expanders is no exception. Patients might face general operation risks such as bleeding, infection, and allergic reactions to anesthesia. It’s crucial for individuals to discuss these potential complications with their healthcare provider beforehand.
Understanding the complication rates is a key step in preparing for surgery. Although most patients undergo this procedure without severe issues, being aware helps in making informed decisions.
Specific Risks
Breast reconstruction introduces specific challenges beyond those of general surgery. One notable risk involves fluid accumulation around the expander, known as seroma. This condition can delay healing and increase the risk of infection.
Moreover, there’s a small risk of developing anaplastic large-cell lymphoma (ALCL), particularly associated with certain types of implants. While rare, this complication underscores the importance of thorough disclosure between patient and surgeon about all potential risks.
Aesthetic Outcomes
Beyond health-related complications, patients should also consider the impact on aesthetic outcomes. The use of tissue expanders allows for gradual breast reconstruction, which can lead to more natural-looking results. However, achieving the desired appearance may require multiple procedures and adjustments.
Summary
Breast reconstruction with tissue expanders is a journey that demands careful planning, understanding, and management. From choosing the right implant to navigating recovery, each step plays a crucial role in achieving your desired outcome. It’s essential to stay informed about the operation process, post-op care, and potential complications. Equipped with knowledge, you can make empowered decisions for your health and well-being.
Remember, this path is uniquely yours. Seeking professional advice and sharing your concerns with your surgeon can significantly enhance your experience and results. If you’re considering breast reconstruction, take the next step. Reach out to a specialist today and explore how you can reclaim your body’s appearance with confidence. Your journey to recovery and self-confidence starts with that first conversation.
Frequently Asked Questions
How do I choose the right implant for breast reconstruction?
Choosing the right implant involves considering factors like size, texture, and material. Your surgeon will guide you based on your body type and desired outcome.
What should I expect when preparing for surgery?
Expect pre-surgical assessments, discussions on risks and benefits, and instructions on fasting or medication adjustments before the operation.
Can you explain the process of breast reconstruction with tissue expanders?
The operation involves placing a tissue expander beneath your skin and chest muscle. Over time, it’s gradually filled with saline to stretch the skin, making room for the final implant.
How do I manage post-op care at home?
Post-op care includes managing pain, monitoring for signs of infection, and adhering to activity restrictions to ensure proper healing.
What are the key points in navigating recovery and activities post-surgery?
Prioritize rest, avoid strenuous activities, and follow your surgeon’s guidelines on gradually resuming physical activities to ensure optimal recovery.
When is exchange surgery planned after tissue expansion?
Exchange surgery is typically planned several months after the initial placement of tissue expanders, allowing enough time for skin expansion.
What options are available for nipple reconstruction?
Options include tattooing for a natural look or surgical reconstruction using grafts from other parts of your body. Your surgeon can recommend what’s best for you.
How are complications and risks addressed in breast reconstruction?
Your surgical team will inform you about potential complications such as infection or implant failure and discuss how these issues are promptly managed.